
The Nervous System
Imagine the nervous system as a light switch dimmer that controls our stress response and relaxation response. When the stress response is activated, it’s like turning the dimmer up, increasing brightness to help us face immediate challenges with heightened alertness and energy, thanks to the release of adrenaline and cortisol. This reaction is essential for survival in short bursts but can become overwhelming if left unchecked.
The relaxation response works like turning the dimmer down and reducing the brightness to promote calm and recovery. Practices like deep breathing and meditation help activate this response, lowering heart rate and blood pressure, and aiding digestion.
A healthy nervous system can seamlessly switch between being activated and relaxed without getting stuck in either extreme, as indicated by Heart Rate Variability (HRV). This balance allows the nervous system to adjust to different situations effectively to without becoming overwhelmed, thereby promoting overall health and well-being (1).
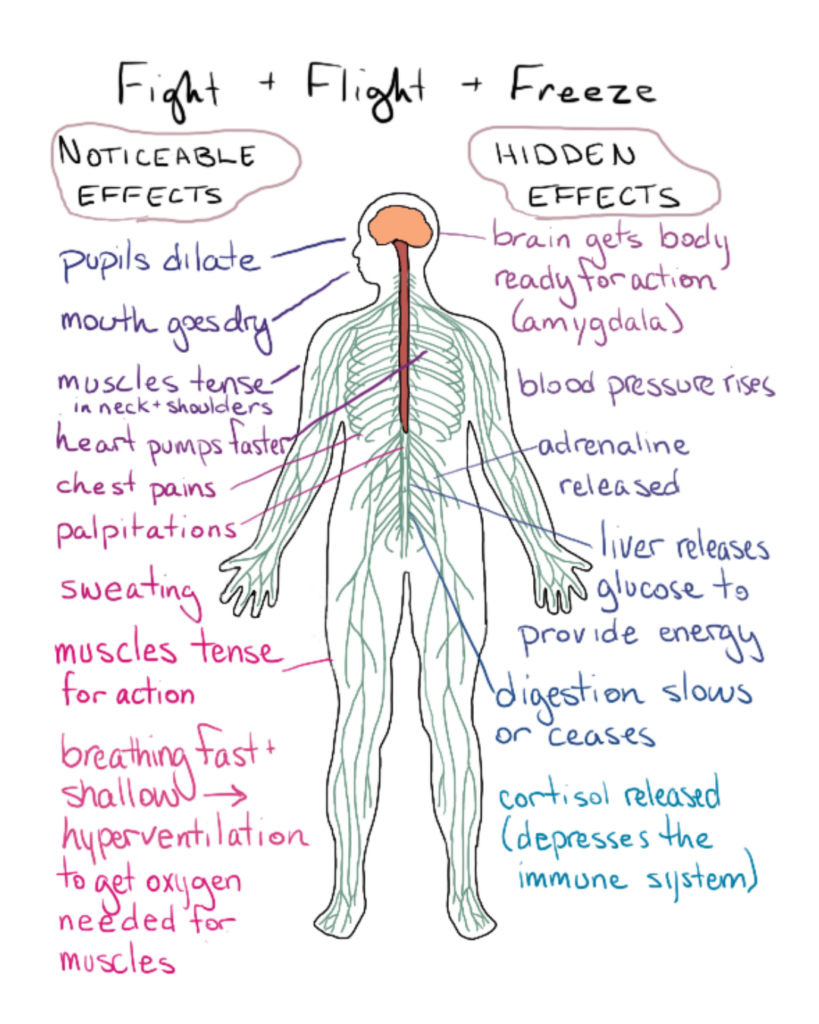
The Stress Response
The sympathetic nervous system, also called the stress response, when activated, triggers a cascade of physiological changes designed to prepare the body for immediate action, often referred to as the “fight or flight” response. This response begins in the brain, where the hypothalamus signals the adrenal glands to release stress hormones, such as adrenaline and cortisol, into the bloodstream (2).
Suppressed Non-Essential Functions: Functions such as digestion, growth, reproduction, and immune responses are temporarily suppressed to redirect energy and resources to deal with the immediate threat (2).
Increased Heart Rate and Blood Pressure: Adrenaline causes the heart to beat faster, pumping more blood to essential muscles and organs, while blood vessels constrict to increase blood pressure, ensuring adequate blood flow to vital areas (2).
HPA Axis: The Hypothalamic-Pituitary-Adrenal (HPA) axis is a central part of the body’s stress response system. The hypothalamus releases corticotropin-releasing hormone (CRH). CRH stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH prompts the adrenal glands to release cortisol. Cortisol increases blood glucose levels by stimulating gluconeogenesis (the production of glucose from non-carbohydrate sources) and by mobilizing glucose stored in the liver (3).
Rapid Breathing: Breathing rate increases to supply more oxygen to the muscles, aiding in quick, efficient energy production (2).
Energy Mobilization: Cortisol raises glucose levels in the blood, providing an immediate source of energy for the muscles and brain (2).
Heightened Senses and Alertness: The brain becomes hyper-focused, improving reaction time and alertness to better respond to potential dangers (2).
Chronic Stress
Stress is not all bad. The way we react to our experiences can have a negative or positive impact on the body and mind. The way we react is the best way we know at this moment with the tools we have. Sometimes, stress can accumulate, which can create chronic stress.
Chronic stress occurs when ongoing, prolonged stressors—stemming from external persistent experiences, negative thought patterns, physiological sensitivities, and environmental factors—persist without adequate periods of recovery or relaxation. Chronic activation of the stress response can lead to numerous health issues, including hypertension, digestive problems, weakened immune function, anxiety, depression, and cardiovascular diseases. Long-term exposure to cortisol can also negatively impact brain function, particularly in areas like the hippocampus, which is critical for memory and learning (2, 4).
Impact of Chronic Stress
Weakened Immune System: Continuous suppression of the immune system can leave the body more vulnerable to infections (5).
Impaired Cognitive Function: Persistent high cortisol levels can damage the hippocampus, an area of the brain involved in learning and memory (4).
Increased Risk of Chronic Diseases: Conditions such as hypertension, heart disease, and metabolic disorders can arise due to sustained high cortisol levels (6).
The Relaxation Response
Just as the stress response ramps up the body’s systems to face challenges, the relaxation response brings the body back to a state of calm. The relaxation response, a term first used by Dr. Herbert Benson, is a state of deep rest that alters the physical and emotional responses to stress. This response is primarily governed by the parasympathetic nervous system (PNS), which promotes the “rest and digest” functions that counterbalance the “fight or flight” reactions of the sympathetic nervous system. When the PNS is activated, it slows the heart rate, decreases blood pressure, reduces stress hormone levels, and promotes digestion and immune function. The vagus nerve, also known as the 10th cranial nerve, is the primary nerve responsible for activating the relaxation response in the body (7).
The Vagus Nerve
The vagus nerve, a vital component of the parasympathetic nervous system, plays a crucial role in the body’s “rest and digest” functions. It extends from the brainstem, travels through the neck and chest, and reaches down to the abdomen, innervating key organs such as the heart, lungs, and digestive tract. By regulating heart rate, blood pressure, digestion, and respiratory rate, the vagus nerve promotes relaxation and recovery, creating a state of calm and balance in the body.
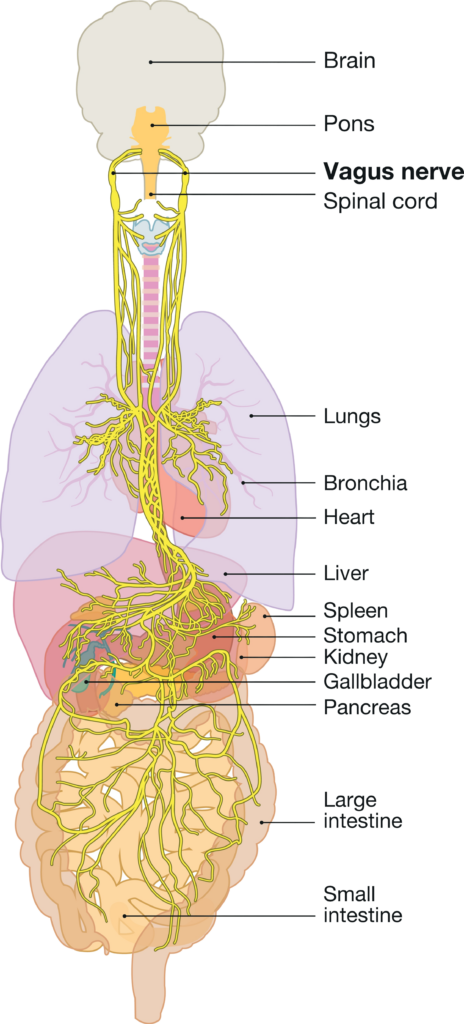
The vagus nerve acts as a vital information highway between the body and the brain. Approximately 80-90% of its fibers are afferent, meaning they carry information from the body to the brain, while the remaining 10-20% are efferent, transmitting signals from the brain to the body. When organs undergo changes, such as the lungs’ stretch receptors located in the walls of the bronchi and bronchioles expanding during a deep breath, the vagus nerve is stimulated and sends a relaxation signal to the brain. Breathing, particularly deep and controlled breaths, is one of the most effective ways to engage the vagus nerve and promote relaxation throughout the body (9, 10).
How to Activate the Relaxation Response
One of the most effective ways to activate the relaxation response is through deep breathing. Slow, deliberate breathing engages the diaphragm, stimulating the vagus nerve. This nerve plays a key role in regulating the parasympathetic nervous system.
Stretch the Lungs: Deep breathing involves engaging the diaphragm, the muscle located below the lungs. When you inhale deeply, the diaphragm contracts and moves downward, creating more space in the chest cavity and allowing the lungs to expand fully. This downward movement of the diaphragm stimulates the vagus nerve, which runs through the diaphragm. The mechanical action of the diaphragm’s movement sends signals via the stretch receptors located in the lung tissue to the brain, activating the vagus nerve. This activation of the vagus nerve promotes a relaxation response, reducing the heart rate and promoting a sense of calm and relaxation throughout the body (11).
Baroreceptor Reflex: Baroreceptors, which are sensitive to blood pressure changes, detect these fluctuations. During deep inhalation, the increased lung expansion slightly decreases blood return to the heart, momentarily lowering blood pressure. When the baroreceptors detect a drop in blood pressure, they send signals to the brain via the vagus nerve. In response, the brain instructs the body to slow the heart rate and widen the blood vessels. This helps to lower resistance to blood flow, maintain stable blood pressure and promote a sense of relaxation and calm (12, 13).
HRV Balance: Slow breathing at six breaths per minute has been shown to optimize Heart Rate Variability (HRV), which is a measure of the variation in time between heartbeats. HRV is an indicator of the balance between the sympathetic nervous system (fight or flight) and the parasympathetic nervous system (rest and digest). Breathing at a rate of six breaths per minute maximizes respiratory sinus arrhythmia (RSA), promoting relaxation and cardiovascular efficiency. RSA is a natural increase in heart rate during inhalation and a decrease during exhalation. Slow breathing enhances RSA, which is associated with a more efficient cardiovascular system and reduced stress (14).
O2 + CO2 exchange: When we breathe, oxygen (O2) enters the lungs and passes through the alveoli, which are tiny air sacs where gas exchange occurs. Oxygen-rich air diffuses across the alveolar membrane into the surrounding capillaries and binds to hemoglobin in red blood cells, creating oxygen-rich blood. The partial pressure of oxygen (PaO2) in the alveoli is higher than in the blood, driving this diffusion. Simultaneously, carbon dioxide (CO2), a waste product of cellular metabolism, diffuses from the CO2-rich blood into the alveoli due to its higher partial pressure in the blood. During exhalation, CO2 is expelled from the body, completing the gas exchange cycle. These pressure changes facilitate the exchange of O2 and CO2, which is essential for maintaining the body’s pH balance, providing oxygen for cellular functions, and removing metabolic waste (15, 16).
The Practice
- Deep Breathing: Engaging the diaphragm through deep breathing stimulates the vagus nerve, activating the parasympathetic nervous system and promoting relaxation. A simple practice involves inhaling slowly for a count of five and exhaling for five, for a total of 6 rounds of breath, all out the nose.
Keep it Balanced
Understanding the stress mechanisms and the relaxation response empowers us to manage our well-being more effectively. By integrating mindfulness techniques such as deep breathing into our daily routines, we can cultivate a stronger parasympathetic nervous system tone. This shift enables us to handle life’s challenges with greater ease and resilience, fostering overall health and well-being. Remember, the nervous system’s adaptability means that with consistent practice, we can rewire our responses to stress and make relaxation our new home base.
Refrences
- Thayer, J. F., & Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders, 61(3), 201-216. doi: 10.1016/S0165-0327(00)00338-4
- Sapolsky, R. M. (2004). Why Zebras Don’t Get Ulcers: The Acclaimed Guide to Stress, Stress-Related Diseases, and Coping. Henry Holt and Co.
- Smith, S. M., & Vale, W. W. (2006). The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues in Clinical Neuroscience, 8(4), 383-395. doi: 10.31887/DCNS.2006.8.4/ssmith
- Lupien, S. J., McEwen, B. S., Gunnar, M. R., & Heim, C. (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10(6), 434-445. doi:10.1038/nrn2639.
- Dhabhar, F. S. (2014). Effects of stress on immune function: the good, the bad, and the beautiful. Immunologic Research, 58, 193-210. https://pubmed.ncbi.nlm.nih.gov/24798553/
- Kivimäki, M., & Steptoe, A. (2018). Effects of stress on the development and progression of cardiovascular disease. Nature Reviews Cardiology, 15(4), 215-229. doi: 10.1038/nrcardio.2017.189
- Benson, H. (2000). “The Relaxation Response.” HarperTorch.
- Galvin, J. A., Benson, H., Deckro, G. R., Fricchione, G. L., & Dusek, J. A. (2006). The relaxation response: reducing stress and improving cognition in healthy aging adults. Complement Ther Clin Pract, 12(3), 186-191.
- Breit, S., Kupferberg, A., Rogler, G., & Hasler, G. (2018). Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 9, 44. doi:10.3389/fpsyt.2018.00044
- Groves, D. A., & Brown, V. J. (2005). Vagal nerve stimulation: A review of its applications and potential mechanisms that mediate its clinical effects. Neuroscience & Biobehavioral Reviews, 29(3), 493-500. doi:10.1016/j.neubiorev.2005.01.004
- Jerath, R., Edry, J. W., Barnes, V. A., & Jerath, V. (2006). Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Medical Hypotheses, 67(3), 566-571. doi:10.1016/j.mehy.2006.02.042
- Ghitani, N., & Chesler, A. T. (2019). The anatomy of the baroreceptor reflex. Cell Reports, 29(13), 3750-3753. doi: 10.1016/j.celrep.2019.11.031
- Joseph, C. N., Porta, C., Casucci, G., Casiraghi, N., Maffeis, M., Rossi, M., & Bernardi, L. (2005). Slow Breathing Improves Arterial Baroreflex Sensitivity and Decreases Blood Pressure in Essential Hypertension. Hypertension, 46(4), 714-718. https://doi.org/10.1161/01.HYP.0000179581.68566.7d
- Joseph, C. N., Porta, C., Casucci, G., Casiraghi, N., Maffeis, M., Rossi, M., & Bernardi, L. (2005). Slow Breathing Improves Arterial Baroreflex Sensitivity and Decreases Blood Pressure in Essential Hypertension. Hypertension, 46(4), 714-718. https://doi.org/10.1161/01.HYP.0000179581.68566.7d
- Habler, O. P., & Messmer, K. F. (1997). The physiology of oxygen transport. Intensive Care Medicine, 23(10), 1031-1050. doi.org/10.1016/S0955-3886(97)00041-6
- Powers, K. A., & Dhamoon, A. S. (2024). Physiology, Pulmonary Ventilation and Perfusion. In StatPearls (Internet). Treasure Island (FL): StatPearls Publishing.